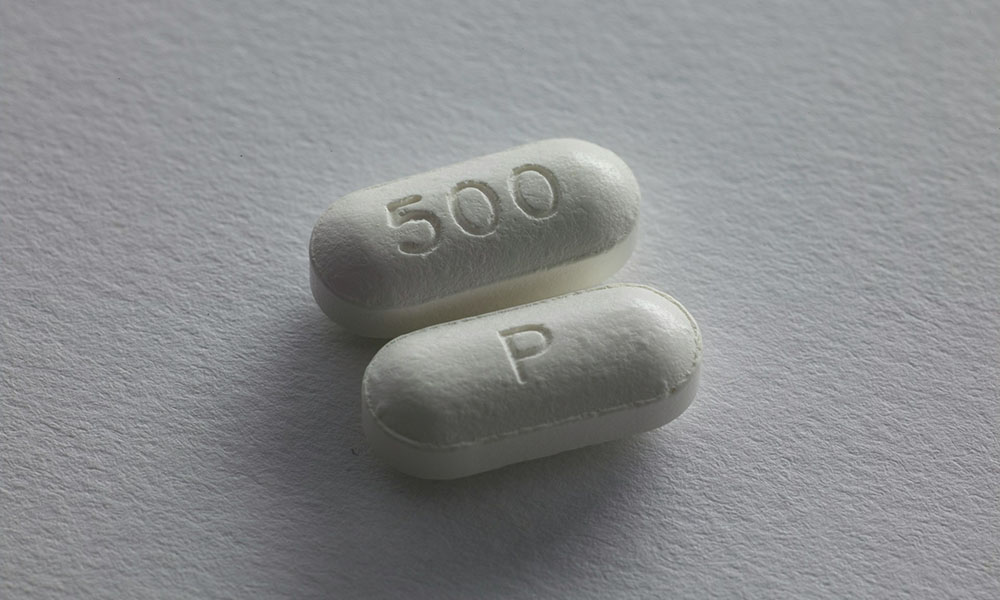
When the U.S. Food and Drug Administration (FDA) announced in October 2025 that approximately 3,000 bottles of Tylenol were being recalled nationwide due to a defective container, the news immediately caught public attention. Tylenol is one of the most widely used over-the-counter pain relievers in the world, trusted by millions of households for decades. A recall of such a familiar product raises urgent questions: Is it safe to keep taking my medicine? How serious is the risk? What should I do if I have a recalled bottle at home?
The answers to these questions lie in understanding the purpose of drug recalls, the FDA’s classification system, and the practical steps consumers can take to protect themselves. Far from being a sign of failure, recalls are actually a vital mechanism for safeguarding public health. They demonstrate that the regulatory system is working to identify risks and remove potentially harmful products before they cause widespread harm.
Why Drug Recalls Matter
A drug recall occurs when a manufacturer, sometimes in coordination with the FDA, removes a product from the market because it violates safety standards or poses a risk to consumers. Recalls can be initiated voluntarily by the company or requested by the FDA. In rare cases, the FDA can mandate a recall under its statutory authority.
The Tylenol recall of 2025 was triggered not by a problem with the drug’s active ingredient, but by a defective container. While this may sound minor, packaging defects can compromise the integrity of a medicine—allowing contamination, incorrect dosing, or accidental misuse. By acting quickly, the FDA and the manufacturer reduced the chance that consumers would be harmed.
Recalls are not meant to create panic. Instead, they are a preventive measure, ensuring that even small risks are addressed before they escalate. In this sense, recalls are a sign of vigilance, not weakness.
Understanding the FDA Recall Classification System
Not all recalls are equal. To help the public understand the level of risk, the FDA uses a three-tier classification system:
- Class I Recall: The most serious type. This classification is used when there is a reasonable probability that using the product will cause serious adverse health consequences or death. For example, a contaminated injectable drug that could cause life-threatening infections would fall into this category.
- Class II Recall: This is the category assigned to the 2025 Tylenol recall. It indicates that using the product may cause temporary or medically reversible adverse health consequences, but the likelihood of serious harm is remote. In other words, the risk is real but not life-threatening.
- Class III Recall: The least severe. This classification is used when a product is unlikely to cause adverse health consequences, but still violates FDA regulations. For example, a labeling error that does not affect safety might trigger a Class III recall.
By assigning recalls to these categories, the FDA provides consumers with a clear signal of how urgent the situation is. A Class I recall demands immediate action, while a Class II or III recall may be less alarming but still requires attention.
What Consumers Should Do During a Recall
When a recall is announced, consumers often feel uncertain. Should they stop taking their medicine immediately? Should they throw it away? The best approach is to follow a few simple steps:
- Check Your Medicine Cabinet
- Look for the specific product, lot number, and expiration date mentioned in the recall notice. Not every bottle of Tylenol—or any other drug—is affected. The FDA and manufacturers usually provide detailed instructions on how to identify recalled products.
- Do Not Panic
- Especially in Class II or III recalls, the risk of serious harm is low. If you have already taken the medicine, the chances of lasting damage are minimal. The recall is a precautionary measure.
- Stop Using the Recalled Product
- If your medicine matches the recall notice, discontinue use immediately. Continuing to take it, even if the risk is small, is unnecessary once the recall has been issued.
- Return or Dispose of the Product Safely
- Many pharmacies accept recalled drugs for safe disposal. Alternatively, follow FDA guidelines for disposing of medications at home, which may include mixing the pills with an undesirable substance (like coffee grounds) and sealing them in a bag before throwing them away.
- Consult a Healthcare Professional
- If you are unsure whether your medicine is affected, or if you have health concerns after taking a recalled product, contact your doctor or pharmacist. They can provide reassurance and suggest alternatives if needed.
- Stay Informed
- The FDA posts recall information on its website and through official alerts. Consumers can also sign up for email notifications. Relying on official sources helps avoid misinformation that may spread on social media.
The Broader Public Health Perspective
The Tylenol recall highlights several important lessons about public health and consumer safety.
First, it shows the importance of regulatory oversight. Without the FDA’s monitoring and classification system, defective products could remain on the market unnoticed, potentially harming thousands of people.
Second, it underscores the role of consumer awareness. A recall is only effective if people know about it and take action. Public communication—through news outlets, pharmacies, and healthcare providers—is essential to ensure that the message reaches those who need it.
Third, it demonstrates the value of trust in institutions. When consumers see that recalls are handled transparently and efficiently, they are more likely to trust both the regulatory system and the brands involved. Conversely, if recalls are hidden or mishandled, public confidence can erode quickly.
A Teachable Moment
The 2025 Tylenol recall may not have been catastrophic, but it serves as a reminder of the delicate balance between convenience, safety, and trust in modern healthcare. For consumers, it is a call to remain vigilant—checking medicine cabinets, paying attention to official notices, and consulting professionals when in doubt. For regulators and manufacturers, it is a reaffirmation of their responsibility to act swiftly and transparently when problems arise.
Ultimately, recalls are not just about removing defective products from shelves. They are about reinforcing a culture of safety, where every precaution is taken to protect public health. In that sense, the Tylenol recall is not merely a story of defective containers—it is a story of a system working as intended, ensuring that even small risks are addressed before they become major threats.
And perhaps that is the most reassuring lesson of all: when the system works, consumers can continue to trust that the medicines they rely on every day are as safe as possible.
